Abstract

Introduction: Cancer survivors, particularly those with hematologic cancers are at increased risk of subsequent malignant neoplasms (SMNs). For survivors of adolescent and young adult (AYA) hematologic cancers, there is a paucity of information on the magnitude and modifiers of SMN risk, as well as outcomes after onset of SMN.
Methods: 1,315 2+y survivors of non-Hodgkin lymphoma (NHL: N=510), Hodgkin lymphoma (HL: N=614), and acute leukemia (Leuk: N=191; 49% ALL, 49% AML), diagnosed at age 15-39y between 1990 to 2012, and treated at Kaiser Permanent Southern California (KPSC) were included in this retrospective cohort study. KPSC is the largest integrated managed care organization in Southern California, with documented 5-year insurance retention rates for AYA cancer survivors approaching 80% (JAYAO 2013 2:59). A non-cancer comparison group (N=17,020) was constructed by selecting KPSC members without a history of cancer individually matched to cancer survivors (1:13) on age at diagnosis, sex, and calendar year. All study subjects were followed from index date until the diagnosis of a malignancy (ascertained using KPSC and California State Cancer Registries), end of 2014, or death, whichever came first. The following analyses were conducted for overall SMNs and solid vs. non-solid SMNs separately: 1) Multivariable Poisson regression adjusting for age, sex, and race/ethnicity to estimate incidence rate ratio (IRR) for SMN comparing cancer survivors to non-cancer comparisons; 2) Cumulative incidence curves of SMN within cancer survivors; 3) Five-year mortality following onset of SMN (survivors) or de novo malignancy (non-cancer comparison); 4) Within cancer survivors, multivariable Poisson regressions to examine the effect of age, sex, race/ethnicity, stage at diagnosis, and radiation exposure on risk of SMNs.
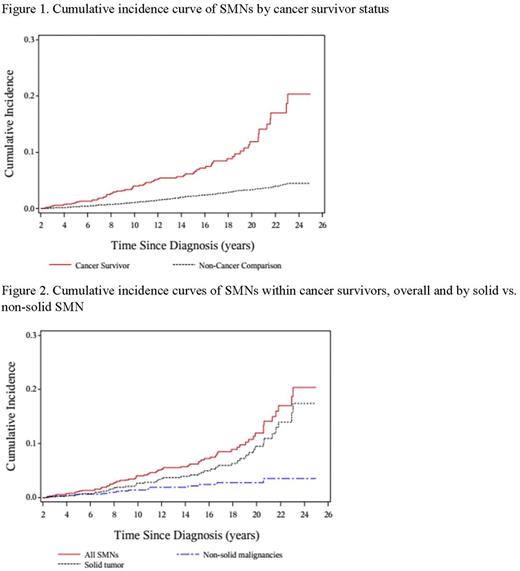
Results: Among cancer survivors, median age at cancer diagnosis was 28y; 51.6% male; 46.2% non-Hispanic white. Median time from cancer diagnosis to end of follow-up was 8.9y (range: 0-23y), representing 11,675 person-years of follow-up. Of the 71 SMNs in cancer survivors, the most common diagnoses were NHL (23%) followed by breast cancer (14%); yet 72% of SMNs were solid tumor. Of the 297 de novo cancer in non-cancer comparisons, 93% were solid tumors. Incidence rate of SMN was 6.08 (7.43 in NHL, 5.66 in HL and 3.91 in Leuk survivors) per 1,000 person-years in cancer survivors. Comparison with non-cancer subjects, a significantly increased risk of SMNs was found in cancer survivors [overall IRR=3.4 (95% confidence interval, 2.6-4.4); NHL IRR=4.0 (2.7-5.9); HL IRR=3.1 (2.1-4.6); Leuk IRR=2.6 (1.1-6.2)]. The overall relative risk was higher for non-solid SMNs: IRR=13.3 (7.3-24.4) than for solid SMN (IRR=2.7 [2.0-3.7]). Cumulative incidence: there was a steep increase in SMN incidence at 18 years after initial cancer diagnosis in cancer survivors (Figure 1), primarily driven by solid tumors (Figure 2). Modifiers of SMN risk within cancer survivors: female sex (IRR=1.88 [1.03-3.43]) and radiation therapy (IRR=1.94 [1.06-3.53]) were associated with increased risk of solid SMNs; while Hispanic race/ethnicity (IRR=0.46 [0.22-0.98]) was associated with lower risk. Black race/ethnicity (IRR=5.30 [1.66-16.97]) was associated with increased risk of non-solid SMNs. Survivors of HL had a lower risk of non-solid SMNs (IRR=0.25 [0.07-0.92]) when compared to those with NHL (referent). Outcomes following malignancy: Five-year overall survival was significantly worse for cancer survivors with solid SMNs when compared to non-cancer subjects who developed a de novo solid tumor after the index date (65% vs. 86%, p=0.02); there was no difference in survival among those with non-solid SMNs (73% vs. 80%, p=1.00).
Conclusion: Survivors of AYA hematologic malignancies are at increased risk of developing SMN when compared to matched non-cancer subjects. In these survivors, there is a steep increase in the incidence of solid tumors >15 years after completion cancer therapy, and certain patient as well as treatment (radiation exposure) characteristics are important modifiers of risk. Among AYA survivors, survival after solid SMN was significantly worse when compared to survival after de novo solid cancer. Taken together these data form the basis for identifying high-risk individuals for population-based targeted surveillance and early screening strategies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal